In this article, you will gain valuable insights into recognizing and addressing breastfeeding jaundice, a common condition that affects newborns. By understanding the signs and symptoms of breastfeeding jaundice, and learning about effective treatment options, you will be equipped with the knowledge to provide the best care for your baby. So, let’s explore this topic together and ensure your little one’s health and well-being!
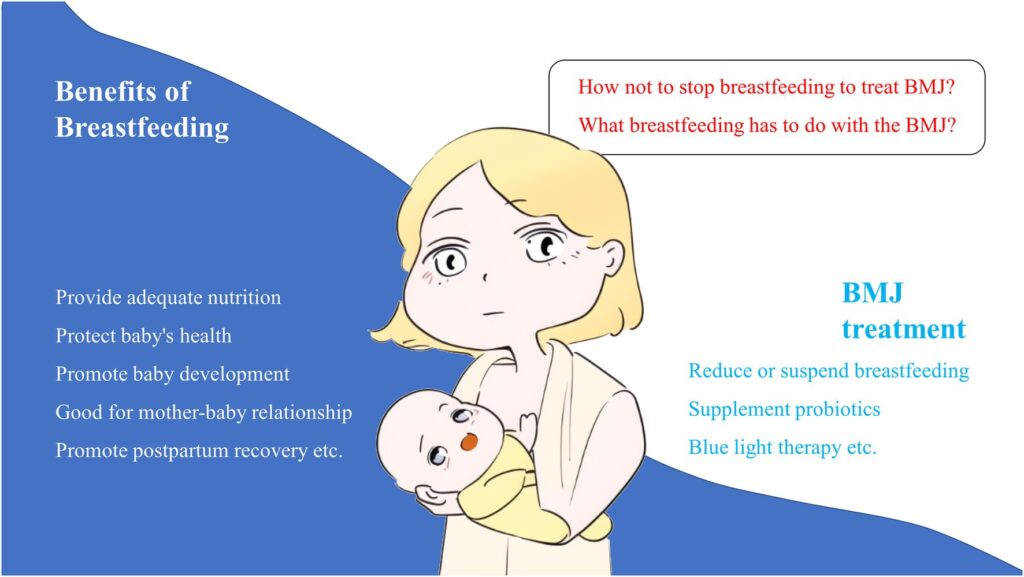
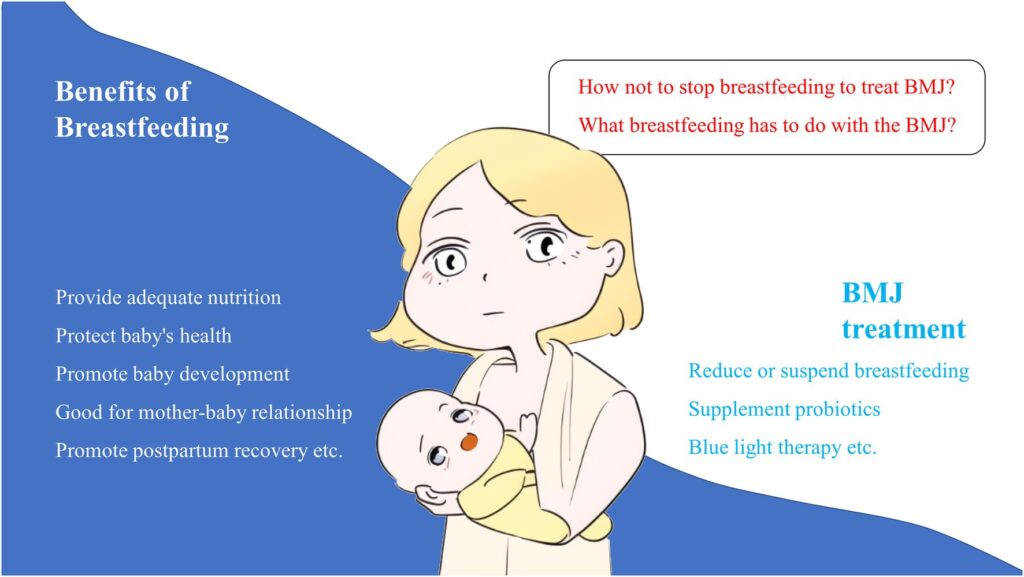
What is Breastfeeding Jaundice?
Definition
Breastfeeding jaundice, also known as breastfeeding-associated jaundice, is a common condition that affects newborns in the first week of life. It occurs when the level of bilirubin, a yellow pigment produced during the breakdown of old red blood cells, becomes elevated in a baby’s bloodstream. Breastfeeding jaundice is typically caused by factors related to breastfeeding and is different from other types of jaundice, such as physiological jaundice or breast milk jaundice.
Causes
Breastfeeding jaundice can be caused by various factors related to breastfeeding. One possible cause is insufficient breastfeeding in the early days after birth. When a baby does not consume enough breast milk, it can lead to a build-up of bilirubin in their system. Another potential cause is inadequate milk transfer during breastfeeding, whether due to latch issues, poor milk supply, or inefficient milk removal. This can result in the baby not receiving enough nutrition and hydration, leading to elevated bilirubin levels.
Risk Factors
There are several risk factors that increase the likelihood of developing breastfeeding jaundice. Premature babies are more susceptible to jaundice due to their immature liver function. Babies with a family history of jaundice or those of East Asian or Mediterranean descent also have an increased risk. In addition, improper breastfeeding techniques, maternal illness, and certain medications can contribute to the development of breastfeeding jaundice.
Recognizing Breastfeeding Jaundice
Symptoms
Recognizing the symptoms of breastfeeding jaundice is crucial for early detection and intervention. The most common symptom is yellowing of the skin and eyes, known as jaundice. However, it is important to note that jaundice can also occur in healthy newborns and does not always indicate breastfeeding jaundice. Other symptoms to watch out for include poor feeding, infrequent urine or stool output, lethargy, and weight loss.
Physical Examination
During a physical examination, a healthcare provider will visually assess the baby’s skin to check for signs of jaundice. They may also use a device called a transcutaneous bilirubinometer to measure the baby’s bilirubin levels non-invasively. Additionally, the baby’s weight will be monitored to assess for any weight loss, which can be an indicator of breastfeeding difficulties.
Diagnostic Tests
In some cases, diagnostic tests may be necessary to confirm the diagnosis of breastfeeding jaundice and rule out other potential causes. A blood test, known as a serum bilirubin test, is the most accurate method to measure bilirubin levels. This test provides healthcare providers with precise information about the severity of jaundice and guides treatment decisions.
Addressing Breastfeeding Jaundice
Breastfeeding Techniques
Improving breastfeeding techniques is an essential step in addressing breastfeeding jaundice. Ensuring a proper latch can facilitate effective milk transfer and prevent nipple pain and damage. Breastfeeding should be initiated as soon as possible after birth, and frequent feeds (at least 8-12 times per day) should be encouraged. Techniques such as breast compression and switch nursing can also be beneficial in increasing milk supply and promoting adequate feeding.
Hydration
Maintaining proper hydration is crucial for newborns with breastfeeding jaundice. Offering the breast frequently and allowing the baby to nurse for as long as they desire helps ensure sufficient fluid intake. Adequate hydration increases the excretion of bilirubin through urine and stool, helping to reduce the bilirubin levels.
Phototherapy
Phototherapy is a common treatment option for breastfeeding jaundice. It involves exposing the baby’s skin to specific wavelengths of light, which helps break down the bilirubin and facilitate its elimination from the body. Phototherapy can be administered using various devices, such as biliblankets or overhead lights. It is a safe and effective treatment method that can significantly reduce bilirubin levels in newborns.
When to Seek Medical Help
While breastfeeding jaundice is usually a benign condition, it is essential to be aware of when to seek medical help. If your baby’s jaundice appears to worsen or if they exhibit signs of dehydration, such as infrequent urination, dry mouth, or sunken fontanelles, it is important to consult a healthcare provider. Additionally, if your baby becomes excessively lethargic or displays signs of acute bilirubin encephalopathy, such as high-pitched cry, abnormal muscle tone, or seizures, immediate medical attention is required.


Prevention of Breastfeeding Jaundice
Early Initiation of Breastfeeding
Initiating breastfeeding as early as possible after birth is an effective preventive measure for breastfeeding jaundice. The colostrum, the nutrient-rich first milk produced by the mother’s breasts, helps promote healthy gut function and facilitates the passage of meconium, the infant’s first stool. By breastfeeding within the first hour of birth, mothers can provide their babies with valuable immunological and nutritional benefits that can help prevent breastfeeding jaundice.
Frequent Feeding
Encouraging frequent feeding is another important preventive strategy. Newborns should be fed on demand, at least 8-12 times in a 24-hour period. Frequent breastfeeding stimulates milk production, ensures adequate hydration, and promotes the elimination of bilirubin through urine and stool. By maintaining a regular feeding schedule, mothers can help reduce the risk of breastfeeding jaundice.
Monitoring Infant’s Stool and Urine
Monitoring the baby’s stool and urine output can provide valuable information about their hydration status and overall health. During the first week, babies should have frequent bowel movements and wet diapers. If the baby’s urine output is significantly reduced or if they have less than three bowel movements a day, it may indicate inadequate intake and potential breastfeeding difficulties that could contribute to breastfeeding jaundice.
Complications of Breastfeeding Jaundice
Although breastfeeding jaundice is generally a temporary and harmless condition, if left untreated, it can lead to complications. Severe and prolonged jaundice can potentially cause a condition known as bilirubin encephalopathy or kernicterus. This rare but serious condition occurs when elevated levels of bilirubin in the blood affect the brain, leading to neurological problems, hearing loss, and developmental delays. Timely recognition and appropriate management of breastfeeding jaundice are crucial to prevent these complications.
Managing Breastfeeding Jaundice in the Hospital
Breastfeeding Support
Providing breastfeeding support to mothers in the hospital setting is essential for managing breastfeeding jaundice effectively. Lactation consultants or trained healthcare professionals can assist mothers with establishing proper latch techniques, ensuring an adequate milk supply, and addressing any breastfeeding difficulties. Their expertise and guidance can help mothers overcome breastfeeding challenges and promote successful breastfeeding.
Supplementing with Expressed Breast Milk
In some cases, supplementing with expressed breast milk may be necessary to ensure the baby’s nutritional needs are met. This can be done through cup feeding, finger feeding, or using a syringe with a soft feeding tube. By providing additional breast milk, the baby’s hydration and caloric intake can be increased, helping to alleviate the jaundice and support healthy weight gain.
Monitoring Bilirubin Levels
Regular monitoring of bilirubin levels is an essential part of managing breastfeeding jaundice in the hospital. Healthcare providers will measure bilirubin levels using blood tests to assess the effectiveness of treatments and interventions. Monitoring allows healthcare professionals to make informed decisions about the need for phototherapy, adjustments in feeding strategies, and when the baby is safe to be discharged.
Support for Parents
Counseling and Education
Counseling and education play a vital role in supporting parents who are navigating breastfeeding jaundice. Healthcare providers can offer guidance on proper breastfeeding techniques, ensuring adequate milk supply, and recognizing signs of sufficient intake. They can provide reassurance, answer questions, and address any concerns parents may have. By providing comprehensive information and emotional support, healthcare professionals can empower parents to make informed decisions for their baby’s health.
Joining Support Groups
Joining support groups can be an excellent source of encouragement and validation for parents dealing with breastfeeding jaundice. Connecting with other parents who have experienced similar challenges can provide a sense of community and foster a supportive environment. Support groups may be available in-person or online, providing a space for parents to share their experiences, seek advice, and gain insights from others who have gone through similar situations.


Conclusion
Breastfeeding jaundice is a common condition that can occur in newborns during the first week of life. It is typically caused by factors related to breastfeeding and is different from other types of jaundice. Recognizing the symptoms, addressing breastfeeding techniques, ensuring hydration, and using phototherapy are essential steps in managing breastfeeding jaundice. Early initiation of breastfeeding, frequent feeding, and monitoring the infant’s stool and urine can help prevent its onset. Timely medical attention and support are crucial to address any complications and promote successful breastfeeding. By providing counseling, education, and support groups, healthcare professionals can empower parents and ensure the well-being of both mother and baby.
